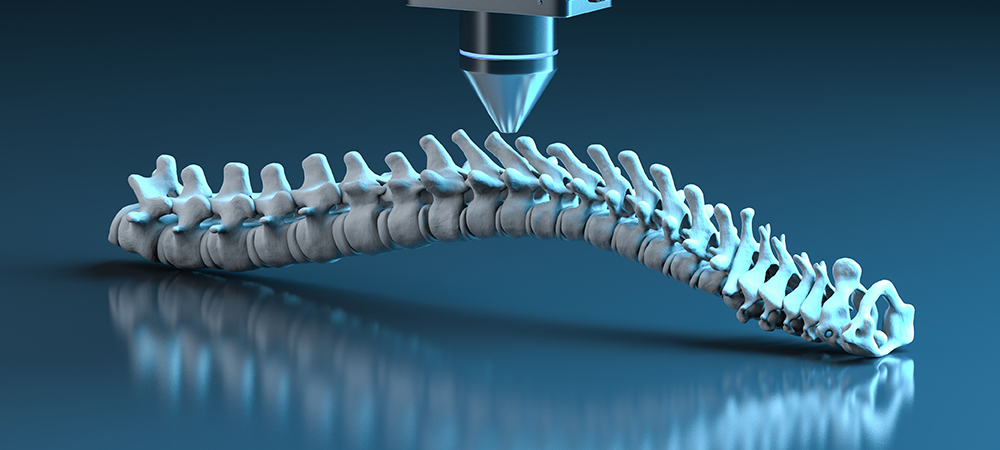
Here, we explore two studies about how the Hospital for Special Surgery (HSS) is using tomography to improve and refine spinal surgeries.
The Hospital for Special Surgery (HSS) is one of the world’s leading medical centres and one of the oldest in the United States, being founded in 1863.
Headquartered in New York, the hospital performs more than 32,000 surgical procedures annually, some of the most popular being hip surgeries and knee replacements. For this, advanced technology is needed – which it is a pioneer in.
Here we explore two ongoing studies from HSS about how the company is using 3D imaging and tomography to improve spinal surgeries.
First, we hear how 3D imaging can improve the accuracy of pedicle screw placement in spine surgery, as well as how CT scans and BPRs are helping to assist this…
A study at HSS has found that intraoperative three-dimensional (3D) imaging was superior to two-dimensional (2D) radiographs in confirming the accuracy of pedicle screw placement during spine surgery.
Many spinal surgeries require the use of implants called pedicle screws to stabilise the spine. Precise positioning of these screws is critical for a successful outcome.
“Two-dimensional biplanar radiographs (BPR) have been the gold standard to confirm pedicle screw placement in spine fusion surgery for many years. However, when utilising BPR, there is the potential that a two-dimensional image alone will not properly demonstrate the successful placement of a screw,” said Darren Lebl, MD, a Spine Surgeon at HSS and Principal Investigator of the study. “As an alternative, three-dimensional intraoperative imaging systems are now available, offering improved visualisation.”
Dr. Lebl and colleagues set out to compare the accuracy of BPR versus 3D imaging when assessing intraoperative pedicle screw placement.
“Our study is the first to compare the differences in intraoperative biplanar radiography and 3D imaging for pedicle screw accuracy in thoracic and lumbar cases using robotic technology,” Dr. Lebl said.
Investigators analysed data from 103 patients who underwent spinal fusion by a single surgeon from 2019 to 2022. Pedicle screw placement was assessed with both intraoperative BPR and 3D imaging in each case.
“CT scans taken after surgery were compared to the findings of intraoperative BPR and 3D imaging to detect either false-positive or false-negative readings,” added Fedan Avrumova, BS, an HSS Clinical Research Coordinator. “False positive findings are instances when BPR imaging suggests the screw was not in an acceptable position, while in fact a more advanced 3D image (intraoperative 3D scan or postoperative CT scan) showed the screw to be in an acceptable position.
“Conversely, a false negative instance was when a BPR image led one to believe or looked as though the screw was in an acceptable position, when in fact a more advanced 3D image or post-operative CT scan showed that it was in fact not acceptable.”
Postoperative CT imaging revealed a clinically significant number of patients who had false-negative and false-positive screw placement readings on BPR. However, screw position shown on intraoperative 3D imaging was found to be much more accurate.
“Based on our study, BPR imaging may lead one to think a screw is acceptable when in fact it is not and also may miss many screws that are not in fact acceptable. In our study, it was approximately 1% of cases where this occurred. However, for surgeons and centres that implant hundreds and thousands of screws per year, this is going to result in a significant clinical impact for many people,” said Dr. Lebl.
“Even one misplaced screw can have a significant impact on a patient, a surgeon and a hospital system. Therefore, based on these findings, we suggest that for intraoperative confirmation of screw position 3D imaging may soon represent a new standard of care.”
In keeping with this, an orthopaedic surgeon at HSS has performed the first augmented reality-guided spine surgery in New York State. We now hear more about this technology, as well as 3D imaging and CT scans, is helping spinal advancements…
Frank Cammisa, MD, Chief Emeritus of HSS Spine, performed a successful spinal decompression and fusion on a 28-year-old male patient with the first augmented reality (AR) system cleared by the FDA for navigation in spine surgery.
Augmented reality refers to digital information that is superimposed on a user’s view of the physical environment, providing images that can’t be seen with the naked eye. AR navigation in spine surgery superimposes 3D images of a patient’s anatomy onto the surgeon’s view of the operative field. Critical elements include a preoperative CT scan of the patient’s spine – which is used to plan and perform the surgery – and an augmented reality headset worn during the procedure.
The system Dr. Cammisa uses consists of a near-eye-display headset and the elements of a traditional navigation system. During surgery, it accurately determines the position of surgical instruments in real-time and superimposes them on the patient’s CT data. It has been likened to giving surgeons ‘x-ray vision’, enabling them to see structures underneath the skin.
“The technology allows us to visualise the patient’s 3D spinal anatomy during surgery to accurately guide instruments and place surgical implants, such as pedicle screws while looking directly at the patient rather than at a separate computer screen,” Dr. Cammisa added. “Improved control and visualisation of the patient’s anatomy and critical structures can lead to a more precise, efficient surgery and can enhance safety.”
He notes that the technology allows for highly personalised surgeries that can be used for most spinal procedures requiring the use of implants. People with degenerative disc disease, spinal stenosis and spinal deformities may be candidates.
Dr. Cammisa notes that as more surgeries are performed with the augmented reality system, patient follow-up and data collection will enable HSS researchers to compare AR to other technologies used in spine surgery to evaluate outcomes.